Immunization requirements and recommendations for the 2025-2026 school year are based on the Advisory Committee on Immunization Practices (ACIP) and the Centers for Disease Control and Prevention (CDC) recommendations. The current recommended and minimum interval immunization schedules may be found on the CDC webpage. The best disease prevention is achieved by adhering to the recommended schedule. However, if a child falls behind, the catch-up schedule is implemented. To avoid missed opportunities, immunization providers may use a 4-day grace period, in most instances, per age and interval between doses. In such cases, these doses may be counted as valid.
K.S.A. 72 - 6261 - Kansas Statutes Related to School Immunizations Requirements and K.A.R. 28-1-20, published July 19, 2019 in the Kansas Register, defines the immunizations required for school and early childhood program attendance.
Diphtheria, Tetanus, Pertussis (DTaP/Tdap): Five doses required. Doses should be given at 2 months, 4 months, 6 months, 15-18 months, and 4-6 years (prior to kindergarten entry). The 4th dose may be given as early as 12 months of age, if at least 6 months have elapsed since dose 3. The 5th dose is not necessary if the 4th dose was administered at age 4 years or older. A dose of Tdap is required at entry to 7th grade.
• Hepatitis A (HepA): Two doses required. Doses should be given at 12 months with a minimum interval of 6 months between the 1st and 2nd dose.
• Hepatitis B (HepB): Three doses required. Doses should be given at birth, 1-2 months, and 6-18 months. Minimum age for the final dose is 6 months.
• Measles, Mumps, and Rubella (MMR): Two doses required. Doses should be given at 12-15 months and 4-6 years (prior to kindergarten entry). Minimum age is 12 months and interval between doses may be as short as 28 days.
• Meningococcal-Serogroup A,C,W,Y (MenACWY): Two doses required. Doses should be given at entry to 7th grade (11-12 years) and 11th grade (16-18 years). For children 16-18 years, with no previous MenACWY, only one dose is required.
• Poliomyelitis (IPV/OPV): Four doses required. Doses should be given at 2 months, 4 months, 6-18 months, and 4-6 years (prior to kindergarten entry). Three doses are acceptable if 3rd dose was given after 4 years of age and at least 6 months have elapsed since dose 2.
• Varicella (Chickenpox): Two doses are required. Doses should be given at 12-15 months and 4-6 years (prior to kindergarten entry). The 2nd dose may be administered as early as 3 months after the 1st dose, however, a dose administered after a 4-week interval is considered valid. No doses are required when student has history of varicella disease documented by a licensed physician.
Legal alternatives to school vaccination requirements are found in K.S.A. 72-6262.
In addition, to the immunizations required for school entry the following vaccines are recommended to protect students:
Human Papillomavirus (HPV): Two doses recommended at 11 years of age or three doses if the series is started after 15 years.
Influenza: Annual vaccination recommended for all ages > 6 months of age. Number of doses is dependent on age and number of doses given in previous years.
Vaccination efforts by school and public health officials, immunization providers, and parents are key to the success of protecting our children and communities from vaccine preventable diseases. Thank you for your dedication.
Student Health Issues
To prevent illnesses from being transmitted at school, the following guidelines will be used to determine when students may be excluded from school and when they may return.
EXCLUDE | RETURN |
|---|---|
Fever of 100 degrees, with or without other symptoms | Fever free for 24 hours* |
Eyes reddened, inflamed with discharge | Discharge has stopped, or 24 hours after initiating antibiotics, or note from health care provider stating not infectious |
Head Lice | After pediculocide treatment is initiated |
Diarrhea (2 or more loose stools in 24 hours) | No diarrhea for 24 hours* |
Vomiting | No vomiting within 24 hours |
Impetigo | 24 hours after administration of antibiotic (either oral or topical). Cover open wounds. Food handler staff is excluded until lesions are healed. |
Ringworm | After administration of antifungal treatment |
Scabies | 24 hours after treatment or note from health care provider |
Chickenpox | When fever is gone and all lesions are crusted or dried. Children who have not had chickenpox or vaccination may also be excluded from school from days 10-21 following exposure to chickenpox. |
Strep Throat | 24 hours of antibiotic treatment and fever free |
Whooping Cough | Exclude all confirmed cases for 5 days following initiation of antimicrobial treatment and note from healthcare provider |
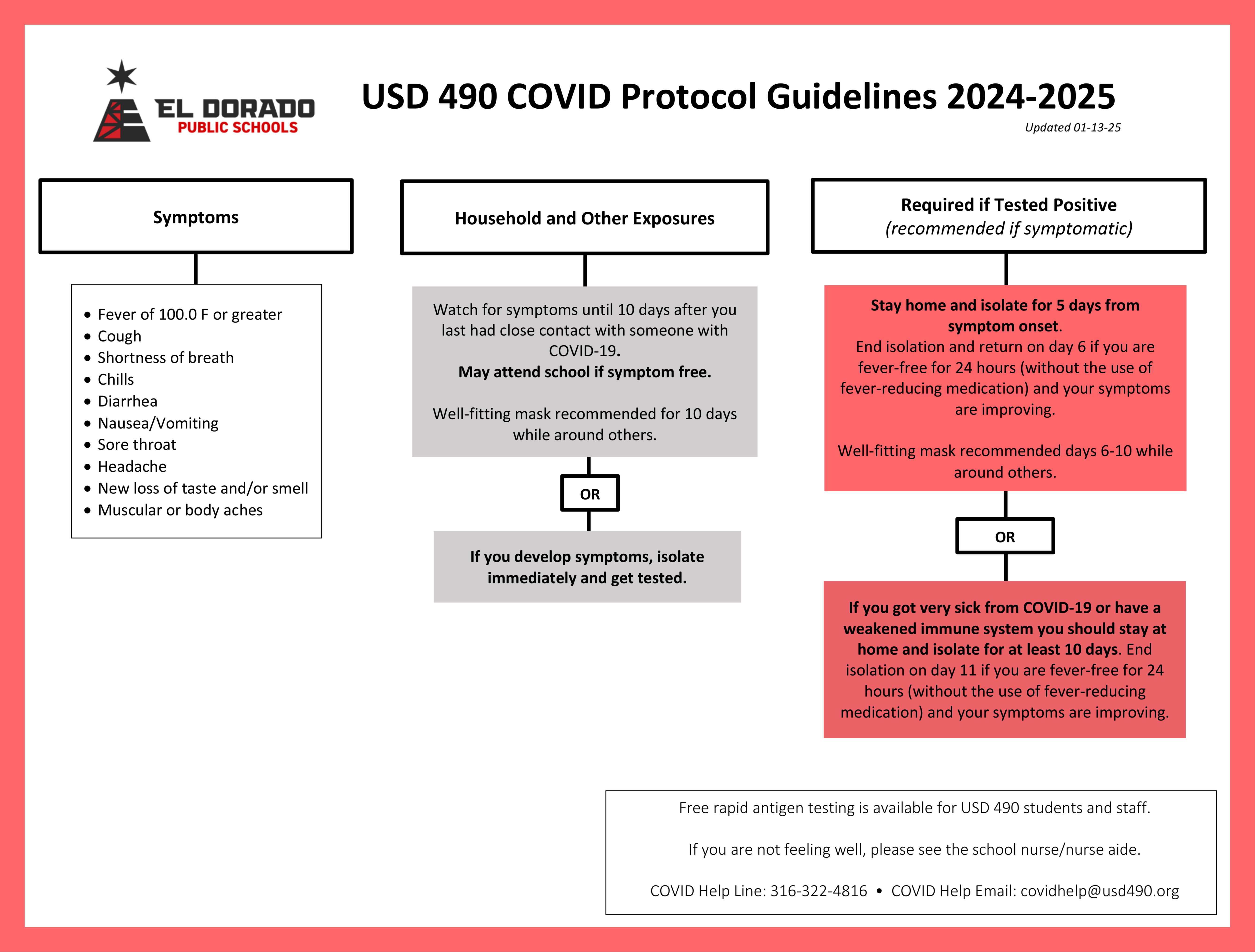
*COVID-19 precautions may require longer exclusion periods.
This is not an all-inclusive list of possible communicable diseases that may impact the school setting. Please call the school nurse if you have questions.
PERTUSSIS (WHOOPING COUGH): Onset 7-10 days, but can occur up to 21 days after exposure to infected person. Pertussis is communicable throughout the incubation period and for approximately 3 weeks following onset if untreated. If treated, infectiousness usually extends 5 days or less after onset of therapy. Symptoms include runny nose, sneezing, low-grade fever, thick mucous, a cough lasting at least 2 weeks with one of the following: inspiratory “whoop” or vomiting after coughing, and exhaustion. If treatment is initiated within 7 days of exposure and no signs or symptoms are present, student may return to school after 24 hours of antibiotic therapy. If symptoms are present and no treatment is initiated the student is excluded for 21 days after exposure and symptoms subside. Students not current with immunization guidelines will be excluded from school for 21 days after exposure and must have a physician’s release to return to school thereafter.
What is Petussis?
Pertussis is a highly contagious respiratory disease. It is often mild in older children and adults; however, in younger children it can lead to complications including pneumonia, inflammation of the brain and in rare cases death.
What are the symptoms of Pertussis?
The early symptoms of pertussis often begin like a cold, with a runny nose, sneezing, fever and cough. The cough lasts 1-2 weeks and gradually becomes worse. The next stage of pertussis includes uncontrolled coughing spells followed by a whooping noise when a person breathes in. During these sever coughing spells, a person may vomit, or their lips or face may look blue from a lack of oxygen. Between coughing spells, a person may appear well. This stage usually lasts 4-6 weeks. Very young infants (<6 months of age), adolescents and adults may not have these symptoms.
Who gets Pertussis?
Pertussis can occur at any age, but is most common in children less than 1 year of age.
How is Pertussis spread?
The bacteria are found in the mouths, noses, and throats of infected people. The bacteria are spread in the air by droplets produced during sneezing or coughing. Symptoms usually appear 7-10 days after by inhaling these droplets.
How long can a person spread Pertussis?
Pertussis is very contagious during the early stage of the illness and becomes less contagious by the end of 3 weeks. Antibiotics will shorten the contagious period of the illness.
How is Pertussis diagnosed?
A sample of mucus from the back of the nose must be taken during the early stage of the illness in order to grow the bacteria. Laboratory tests can be done on the sample to identify the bacteria.
How is Pertussis treated?
Infants less than 6 months of age and persons with severe cases often require hospitalization and severe cases may require oxygen and mild sedation to help control coughing spells. Antibiotics may make the illness less severe if started in the early stage of the disease.
How can Pertussis be prevented?
•Giving a series of shots to children in early infancy can prevent pertussis. Pertussis vaccine is given at 2, 4, 6, and 15 monthss of age, and again when a child enters school. At least 3-4 doses are necessary to protect a child from pertussis.
•Prompt use of antibiotics in a household is helpful in limiting other cases. In a daycare setting, antibiotics should be given to household contacts and other close contacts. Children who develop symptoms within 14 days of exposure should be excluded from day care until a diagnosis can be made.
Where can I get more information?
• Your local health department
• Kansas Department of Health and Environment, Epidemiologic Services Section (877) 427-7317
• http://www.cdc.gov/health/default.htm
• Your doctor, nurse, or local health center
MUMPS: an infection of the salivary glands caused by a virus. Symptoms include fever, headache, muscle ache, and swelling of the glands close to the jaw. Transmission of mumps occurs through coughing and sneezing by airborne particles, or through direct contact with infected droplets or saliva. Mumps is about as contagious as influenza and rubella, but less so than measles or chickenpox. It is generally transmitted from about 3 days before symptoms appear to about 4 days after, although the virus has been isolated from saliva as early as 7 days before to as late as 9 days after onset of symptoms. Complications of mumps can lead to meningitis, inflammation of the testicles or ovaries, inflammation of the pancreas and deafness (usually permanent).
Exclusion: Persons diagnosed with mumps are excluded from school for 9 days following diagnosis. Those without the compliant immunizations (1 MMR after 12 months of age and a second MMR before entering school) are excluded from school based on a range of days during which exposure could have occurred (i.e., starting the 12th day of exposure following the first day of exposure and extending to the 25th day following the last day of exposure). The MMR vaccination is recommended for all exposed persons who do not have the proper immunizations. Persons born before 1957, or those who have had a confirmed case of the mumps are considered to have immunity